BlackBook gives treatment centers the tools to take control of their financial future. With instant eligibility verification, payer performance insights, and AI-enhanced reporting, every step from admission to reimbursement becomes clear, connected, and predictable.
See how payers actually perform with historical data on collection rates, speed, and out of network behavior.
Track claims and revenue in real time with AI enhanced forecasting that makes revenue predictable.
Instantly verify patient insurance coverage in seconds to reduce delays and keep admissions on track.
Too many organizations operate in silos. Eligibility, reimbursements, and reporting happen in separate systems that never align. Without one connected system, treatment centers lose control of revenue.
Blackbook brings everything together in one platform, giving treatment centers the clarity and control they need to grow.
BlackBook gives treatment centers of any size the clarity to act with confidence. From admissions staff checking benefits, to executives forecasting revenue, every role gains the insights needed to reduce risk and improve outcomes.
Manage a single facility or unify multiple locations within one organization view. Leadership sees performance at every level without spreadsheets.
Add facilities and teams in one place. Keep permissions clean and data consistent.
Drill into one facility or roll up across locations with simple global filters.
Admissions, finance, and leadership work from the same numbers and the same timeline.
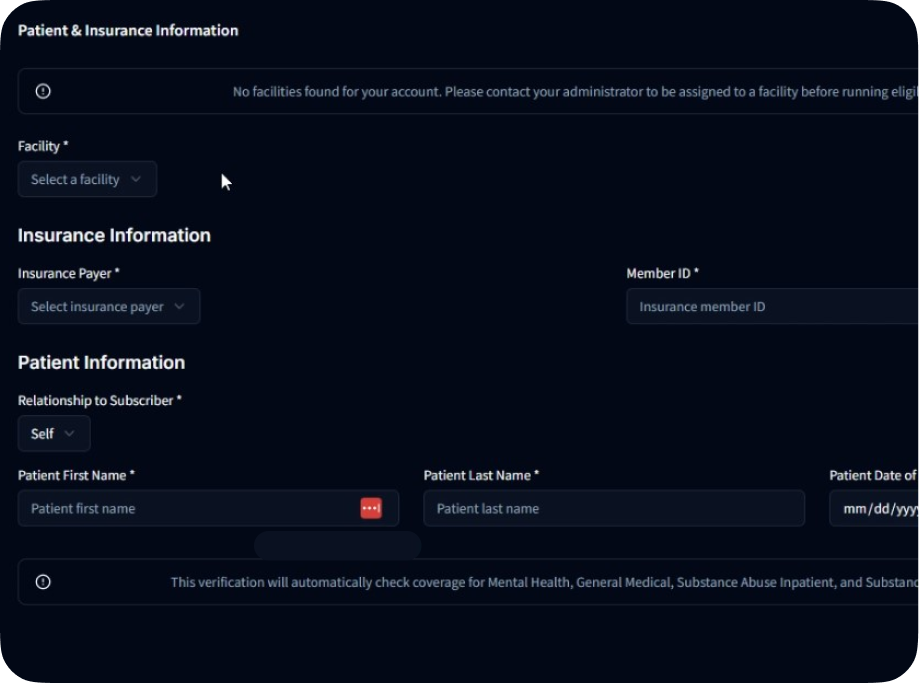
Admissions teams run instant eligibility with BlackBook VOB so patients move forward without delay and claims start clean.
Use demographics, plan, and prefix. Facility defaults and dates save time for your team.
See coverage levels, copays, deductibles, and any authorization requirements for mental health and substance use.
Push verified details forward so finance does not re enter data and denials drop.
Use payer and member ID prefix intelligence to understand likely financial outcomes before admission and during utilization review.
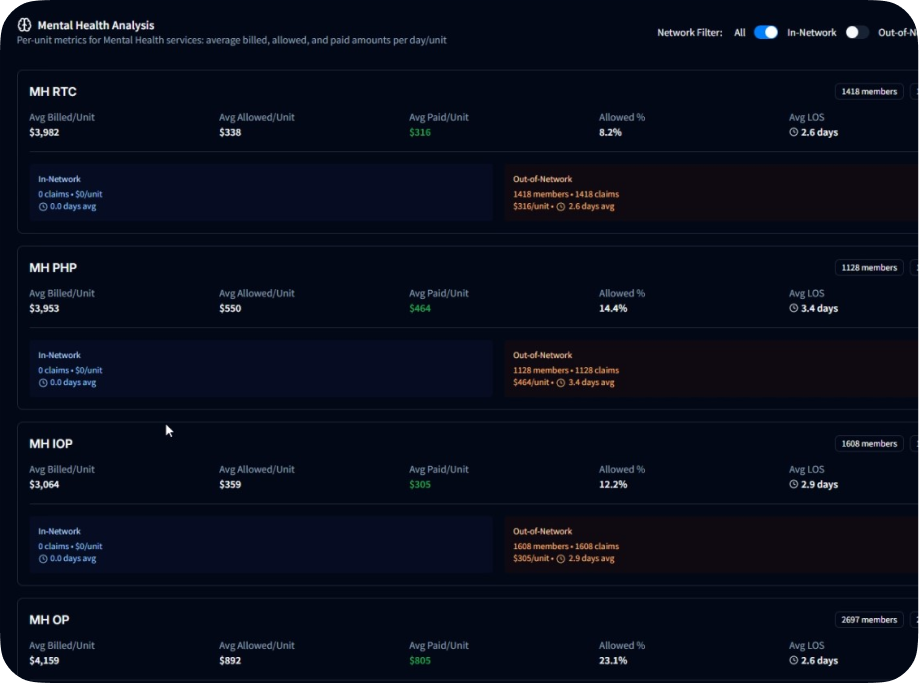
View average billed per unit, average allowed per unit, average paid per unit, and allowed percent by prefix.
Review average length of stay trends that influence revenue planning and authorization strategy.
See in network and out of network behavior across RTC, PHP, IOP, and OP for mental health and substance use.
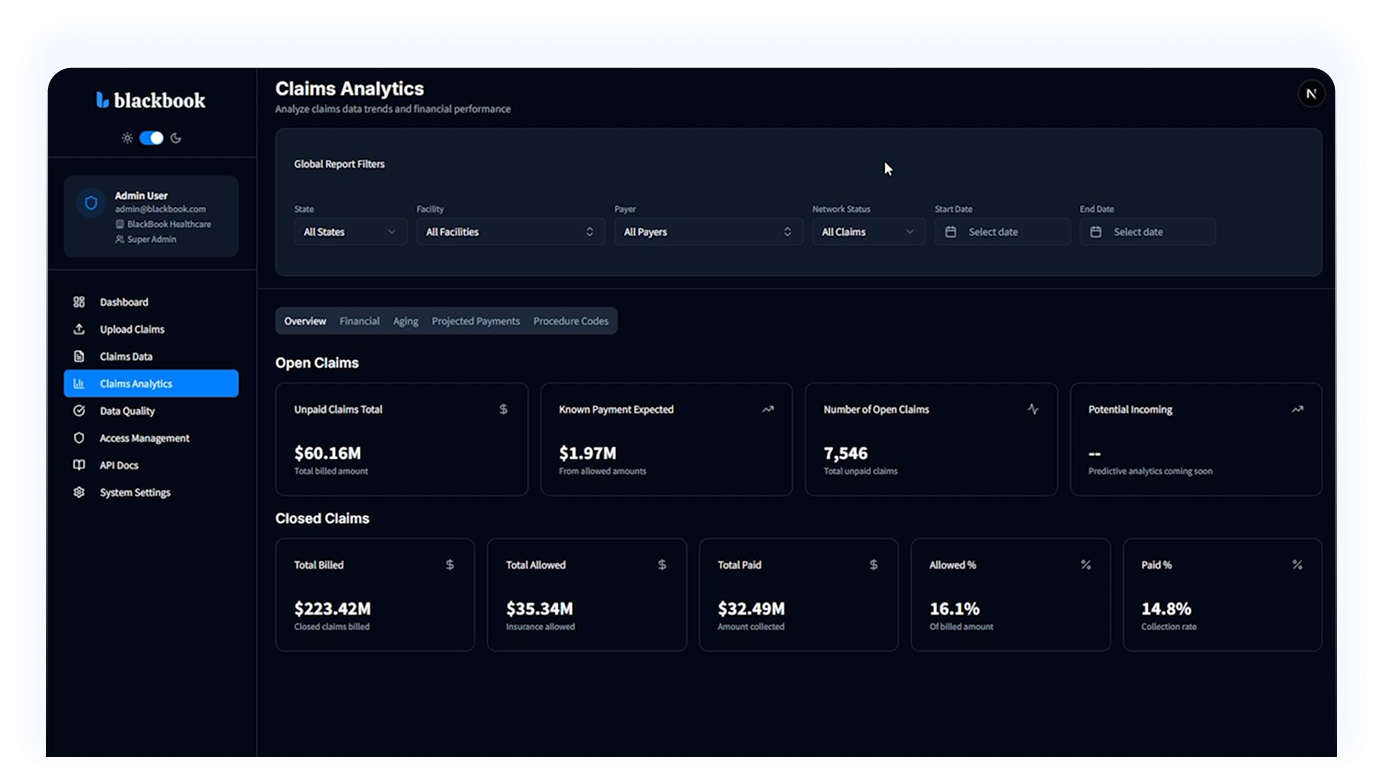
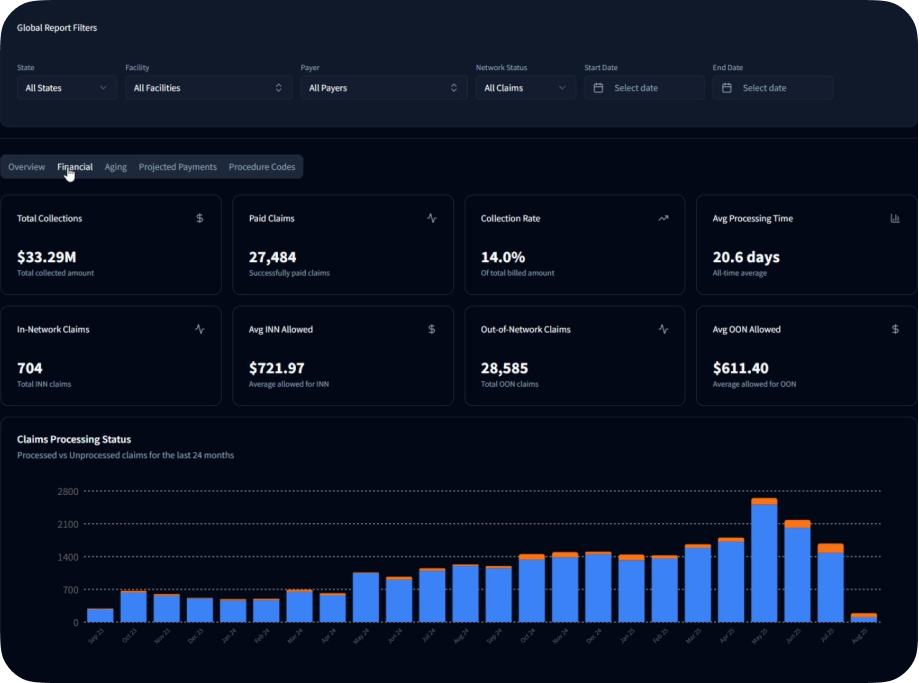
Replace disconnected spreadsheets with real time reporting. Track claims, collections, and code level performance across facilities or in one location.
See aging buckets and collection progress so teams act on the right accounts at the right time.
Review revenue code and CPT performance to catch shortfalls and tighten contracts.
Use global filters to compare facilities or focus on a single program without losing context.
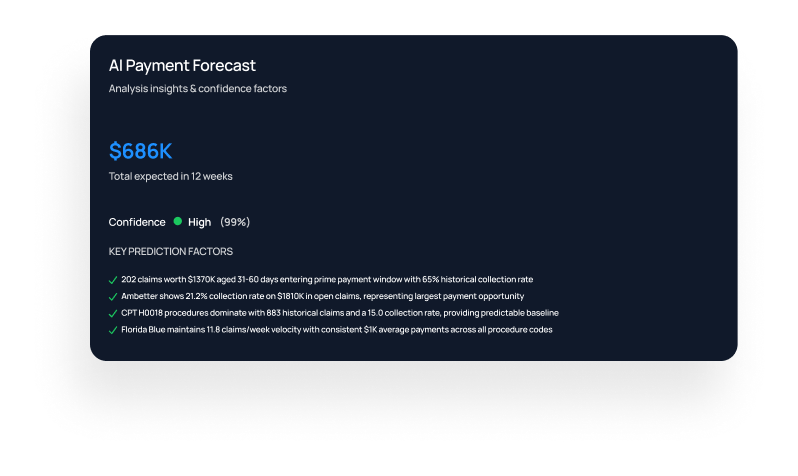
AI powered forecasting projects payments week by week using your historical data and confidence factors so leadership can plan with certainty.
View expected cash in for the next eight to twelve weeks and plan staffing and spend.
Understand which payers and codes are shaping the outlook so you can act early.
Admissions, finance, and executives use the same projections which makes decisions predictable.
Whether you need eligibility, historical payer insights, or both, Blackbook makes it simple. Every plan comes with free reporting when you upload claims data.
Start verifying coverage with ease.
Overages billed monthly: eligibility $1 each
Learn what payers historically paid.
Overages billed monthly: insights $3.50 each
Best value: eligibility + insights together.
Overages billed monthly: eligibility $1 each; insights $3.50 each
Unlock dashboards when you contribute data.
Verify coverage, learn what payers historically pay, and forecast revenue with a single tool.